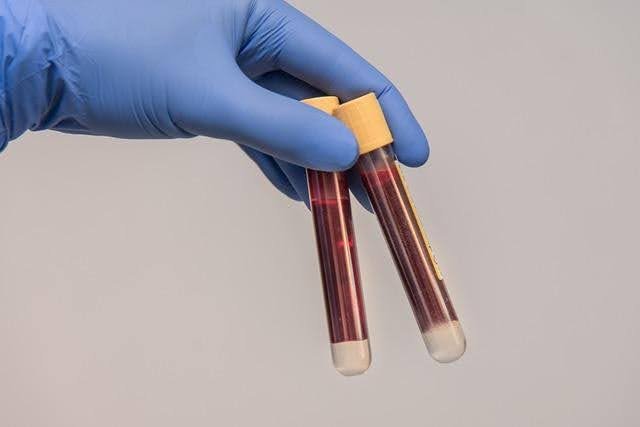
Blood hemolyzing in clinical laboratories disrupts accuracy and increases repeat testing, delaying patient care. When red cells rupture, they alter sample composition and interfere with many assays. Understanding what causes hemolysis helps labs build reliable workflows. With proper technique, clear protocols, and strong quality control, teams can reduce errors, protect sample integrity, and ensure dependable results across all departments.
Why Blood Hemolysis Occurs in Clinical Laboratories
Biological Vulnerability of Red Blood Cells to Stress
Red blood cells are fragile and easily damaged by physical, chemical, or osmotic stress. Their flexible membranes respond poorly to force, temperature shifts, or improper handling. When exposed to harsh conditions, cells lose stability and rupture. Understanding this vulnerability helps clinicians handle samples more carefully, protect cell membranes, and prevent unnecessary hemolysis during routine laboratory workflows and patient care procedures.
Technical Factors That Trigger Cell Rupture
Technical errors such as using small needles, applying excessive suction, or forcing blood through narrow tubing can rupture cells. Improper mixing, vigorous shaking, and delays before processing further increase stress. These actions introduce mechanical forces that red cells cannot withstand. Identifying high-risk techniques allows teams to adjust procedures, reduce handling errors, and maintain better sample quality throughout collection and transport.
Common Workflow Steps Where Hemolysis Happens
Hemolysis commonly occurs during venipuncture, tube filling, transport, and centrifugation. Rough handling, temperature extremes, and prolonged storage increase the likelihood of cell damage. Even routine tasks such as inversion or aliquoting can cause rupture if performed incorrectly. Recognizing these vulnerable steps helps labs reinforce procedures and adopt preventive measures that keep red blood cells intact from start to finish.
Pre-Analytical Practices to Reduce Hemolysis
Proper Venipuncture Technique and Tube Selection
Effective prevention starts with correct venipuncture. Using the right needle size, selecting appropriate tubes, and avoiding excessive force protect cell integrity. Allowing the site to dry fully and ensuring proper order of draw also reduce risk. Well-trained phlebotomists follow precise techniques that minimize stress on red cells and improve the likelihood of collecting clean, hemolysis-free samples every time.
Correct Handling, Mixing, and Transport of Samples
Gentle handling preserves sample quality. Correct inversion techniques prevent clotting without stressing cells. Avoiding tube shaking, preventing air bubbles, and reducing vibration during transport help maintain stability. Timely movement to processing areas prevents degradation. By following controlled handling and transport steps, labs protect the sample from mechanical forces that often lead to hemolysis and inconsistent test results.
Controlling Temperature and Environmental Conditions
Temperature fluctuations weaken red cell membranes. Excessive heat, cold exposure, or repeated cycling increases fragility and leads to hemolysis. Maintaining stable environmental conditions during storage and transport helps safeguard samples. Lab teams monitor temperature ranges, avoid prolonged outdoor exposure, and use insulated carriers when needed. Controlled environments reduce cell damage and help maintain reliable sample composition for analysis.

Analytical and Post-Analytical Considerations
Avoiding Excessive Mechanical Stress During Testing
Analytical instruments may create pressure, vibration, or shear forces that damage cells if settings are incorrect. High-speed mixing, rapid aspiration, or unbalanced centrifugation increase rupture risk. Adjusting equipment settings and maintaining proper balance protects samples. By monitoring mechanical forces throughout processing, labs minimize hemolysis and preserve accurate values for chemistry, hematology, and diagnostic assays.
Monitoring Instrument Parameters That Influence Hemolysis
Instrument parameters such as pump speed, probe depth, and centrifugation force affect cell stability. Incorrect calibration or worn parts can introduce stress that causes hemolysis. Routine maintenance helps detect issues early. Monitoring instrument performance ensures consistent sample handling and prevents equipment-related cell damage. Reliable parameters support accurate test results and reduce unexpected variability across analytical workflows.
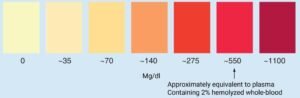
Effective Identification and Management of Compromised Samples
Early identification of hemolyzed samples prevents reporting inaccurate results. Visual inspection, hemolysis indices, and automated flags help detect compromised specimens. Clear rejection criteria guide decisions on recollection or additional review. Managing compromised samples prevents misleading data from reaching clinicians and maintains confidence in laboratory reporting. Effective evaluation ensures only high-quality samples proceed to analysis.
Quality Programs That Strengthen Hemolysis Prevention
Training Staff to Recognize High-Risk Procedures
Education empowers staff to understand how their actions affect sample integrity. Training highlights risky procedures, proper venipuncture, and best handling techniques. Simulation exercises and competency checks reinforce skills. When teams recognize behaviors that trigger hemolysis, they adjust routines and maintain higher standards. Ongoing education builds confidence, improves performance, and reduces errors across all laboratory shifts.
Standardizing Protocols Across All Shifts and Teams
Standardized protocols ensure everyone follows the same steps, reducing variability that leads to hemolysis. Clear instructions for collection, transport, mixing, and centrifugation help maintain consistency. Documentation supports accountability and smooth transitions between shifts. When every team uses aligned practices, the entire laboratory benefits from fewer errors, improved efficiency, and more reliable sample quality.
Using Continuous Audits to Improve Prevention Rates
Audits help labs track hemolysis trends, identify recurring issues, and evaluate protocol compliance. Regular review of indicators such as hemolysis index rates guides corrective actions. Data-driven interventions strengthen weak areas and support ongoing improvement. Continuous auditing builds a proactive culture focused on quality, ensuring sustained reductions in hemolysis and better outcomes for patients and clinicians.
Conclusion
Preventing blood hemolyzing in clinical laboratories requires strong technique, consistent protocols, and clear attention to sample handling. When teams understand where hemolysis occurs, they apply effective safeguards that protect red cells from stress. Quality programs and training reinforce good practices, while monitoring catches issues early. A prevention-focused approach ensures accurate testing, fewer recollections, and reliable results for patient care.